“I’m really glad you’re finally opening up,” the counselor says gently, “but I’m afraid this is our last session.” Wait—last session? After just three hour-long conversations, Nina isn’t “fixed.” In fact, she’s only scratched the surface of her burnout and anxiety. Session 4 won’t happen – at least not through her company’s Employee Assistance Program (EAP). Nina forces a smile, gathers her coat, and wonders what now? This scene (or some version of it) unfolds in offices worldwide, leaving employees and HR leaders alike asking a crucial question: Your EAP offers 3 sessions. What happens on session 4?
The Three-Session Conundrum: A Band-Aid on a Bullet Wound
Most traditional EAPs cap therapy at 3 to 6 sessions per issue[1], with three sessions being a common offering. The intent is noble – provide short-term counseling to help employees through a tough spot[2]. But for many modern woes, three therapy sessions are like putting a band-aid on a bullet wound. Consider this: research shows most people need 15–20 sessions of therapy for meaningful improvement, yet EAPs provide just 2.5 sessions on average[3]. That’s a startling gap. It means employees often hit a hard stop just as they begin to gain trust and momentum with their counselor.
“I only just started to heal, and then the help was gone,” confided one employee after exhausting her EAP sessions.
At session 1, you’re a stranger to yourself; by session 3, you’re finally unpacking real issues – and then, poof, the free support vanishes. No wonder it feels abrupt and even emotionally jarring. One clinician noted how hard-won trust is fragile; in a real intake, a therapist had to deeply attune to a client’s cultural background just to help her open up[4]. Imagine building that trust and then telling the person, “Glad you shared… but our time is up forever.” For employees already hesitant to seek help, this can feel like a door slamming shut right when they needed it to stay open.
People don’t heal on a company deadline. Yet the three-session model can unintentionally send the message that there’s a quick fix for burnout, grief, or depression. The truth? These struggles are complex, and a few hours of counseling often only reveal the tip of the iceberg. As one intake case revealed, a client sobbed that she “hadn’t left [her] room in 5 weeks” after a decade-long relationship imploded[5]. Three sessions might barely get her from crisis to stable, but certainly not to whole. EAP counselors do their best within these constraints – focusing on assessment, a bit of support, and then referral out to longer-term care. But many employees never follow through on that referral. Why? Because life comes rushing back in, or because finding affordable, convenient care beyond EAP is its own daunting journey.

EAP Effectiveness in 2025: Beneath the Low Utilization Rates
Before we even get to session 4, there’s another elephant in the room: EAP utilization is abysmal. It’s ironic – in an age where nearly 90% of large employers offer EAPs, only a single-digit percentage of employees ever use them[6]. In the U.S., EAP utilization hovers around 5–7% on average[6]; in the UK it’s similarly about 5%, with the majority of employees never dialing that counselor number[7]. Reasons vary: stigma, lack of awareness, and mistrust top the list[8]. Many employees fear that tapping EAP support could mark them as “weak” or jeopardize their job, despite assurances of confidentiality. Others simply forget the EAP exists until they’re in absolute crisis.
And here’s a startling insight: even when employees do reach out, many don’t receive actual counseling. Data from EAP providers show that 60% of initial calls are redirected to self-help resources or external charities (in other words, “Here’s a website or hotline, good luck”)[7]. Only about 40% of callers get referred to a counselor at all, often with the onus on the employee to follow up and schedule that session[7]. The result? By the time a person finally sits down for Session 1, they might have already jumped through hoops – when they’re likely at their most drained and vulnerable.
So yes, EAPs have an effectiveness problem in 2025. They were a great idea (and they do help some people), but they haven’t evolved fast enough for today’s mental health landscape. Burnout, anxiety, and depression are at all-time highs – yet the old-school EAP model isn’t fully delivering. One HR survey found that 82% of employers thought they were supporting mental health, but only 50% of employees agreed[9][10]. There’s a clear disconnect. Employers are pouring money into EAPs (often as a check-the-box benefit), but employees aren’t feeling the impact where it counts.
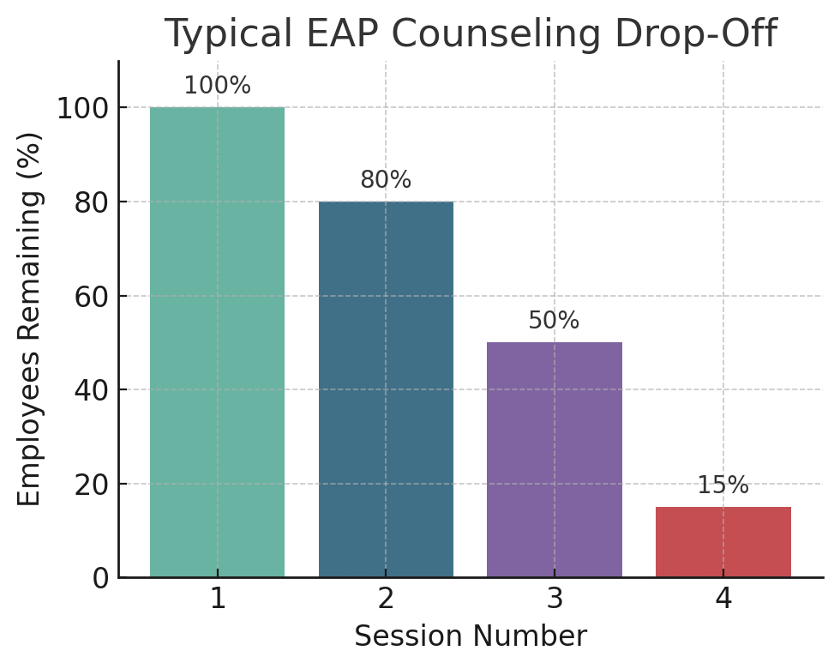
Why does this happen? Partly, it’s by design: EAPs were never meant as long-term therapy – they originated as a first line of defense, a triage. EAP counselors often address immediate issues (stress, a conflict, a substance use flare-up) and then point the person to longer-term resources. But in practice, employees often treat the EAP as one-and-done, either because they got what they needed in those few sessions (rare, but it happens), or because transitioning to another therapist for session 4 feels like starting over. It’s the equivalent of pouring your heart out to a stranger three times and then being handed a list of “in-network providers” to cold-call on your own. Many just… give up at that point. The follow-through drop-off is huge.
To be fair, EAPs can claim some victories. Studies show they do improve short-term outcomes for many who use them – reduced depression scores, lower absenteeism, etc.[11][12]. But those successes are typically among the fraction who both used the EAP and likely had relatively mild or situational issues that brief counseling could resolve. For more complex or chronic challenges (think: serious burnout, trauma, ongoing mental health disorders), a few sessions are just not enough to move the needle long-term. Even EAPA UK’s Chair, Eugene Farrell, acknowledged that EAPs “have their limits” and are not a panacea for deep-seated problems[13].
Burnout in 2025: An Epidemic No Three Sessions Can Cure
Let’s talk about burnout, one of the biggest threats to workplace well-being today. This isn’t the “I had a long week” tired; it’s the soul-deep exhaustion and cynicism that builds up over months or years. By mid-2025, reports showed job burnout at 66% – an all-time high[14]. Two-thirds of employees are running on fumes, many barely hanging on. Burnout sneaks up until, suddenly, an employee is crying in their car before work or feeling physically ill on Sunday nights.
Now, imagine telling a burnt-out employee: “Good news, we have resources! You can talk to a counselor… up to three times.” 🙄 It almost sounds like a punchline. Burnout recovery requires real, sustained intervention. According to the World Health Organization, fighting burnout involves organizational change (like adjusting workloads and expectations) and personal change (learning resilience skills, possibly therapy, definitely rest). None of that fits neatly into three 45-minute chats.
Think of burnout like a forest fire: EAP counseling is a quick water drop – it might dampen the flames temporarily, but without continuous effort the fire will rage again. One senior manager, after using an EAP, joked bitterly that “they gave me a couple of breathing exercises and sent me back into the wildfire.” That dark humor underscores a truth: Employees often feel tossed back into the same environment that burned them out, with too little support to navigate it differently.
So what would meaningful burnout support look like? For starters, more time to process and heal. Burnout often involves unlearning habits of overwork and guilt, redefining boundaries, and rekindling one’s sense of purpose. Those are tall orders that unfold over weeks and months. A skilled therapist can help, but not under a three-session cap. It’s like telling someone with a broken leg that you can only offer three physical therapy sessions—after that, they’re on their own to finish healing.
This is where employee mental health tools beyond traditional counseling come in. In 2025, progressive companies aren’t just handing out an EAP brochure and hoping for the best; they’re looking at workplace well-being holistically. That means tackling burnout on multiple fronts: workload adjustments, manager training, and innovative mental health resources that employees can access anytime. Apps for guided mindfulness, virtual support groups, self-paced learning modules on stress management – these employee mental health tools act as continuous support systems. They don’t replace therapy, but they can extend and supplement it in between or after live sessions.
The Emotional Cliff at Session 4: Why Many Don’t Continue (and What It Costs Us)
Let’s circle back to “Session 4” – the session that never happened for so many. Why don’t more people continue counseling after EAP referrals? Often, it’s financial or logistical barriers. The EAP might refer Nina to an external therapist, but then Nina learns it’ll be a $50 copay per session (or worse, she’s out-of-network and it’s $150). Maybe she’ll have to wait three weeks for an opening – by then, her motivation wanes. Or maybe she really liked her EAP counselor and doesn’t relish starting over with someone new, recounting her entire painful story from scratch. Therapeutic relationships take time to build, and switching providers can feel like a setback.

There’s also a psychological effect: relief followed by relapse. After three sessions, an employee might feel a bit better – crisis triaged, emotions validated. The urgency dips, so they might postpone seeking further help… until a few months later when things crumble again. It’s a classic boom-and-bust cycle in mental health care. We see it in intake trends: clients who come to therapy say they tried EAP last year, felt improvement, but didn’t stick with it. Now the burnout or depression is back full force, and they regret not having continuous support. One Reddit user summed it up: “I get four free EAP sessions and probably won’t continue therapy after that because I can’t afford it.” That sentiment is more common than we’d like to admit.
The cost of this drop-off isn’t just personal – it’s organizational. Employees who almost got help but didn’t fully resolve their issues can end up in a holding pattern of struggle, which translates to lower productivity, more sick days, or even quitting the job. From HR’s perspective, it’s painful: you invest in an EAP to help your people, but if the help is too short-lived, the ROI evaporates. Studies have found that while EAPs claim positive ROI (like one report of £8 return per £1 invested in the UK[15]), those figures assume employees actually complete treatment and get better. In reality, incomplete care can mean a false start – the employee’s downward spiral is paused, not halted.
Culturally, there’s an element of trust at stake too. If employees feel the company’s support is transactional (“we’ll pay for three sessions, then you’re on your own”), it can erode trust in leadership’s platitudes about caring for employee wellbeing. On the other hand, when employees see that their organization understands the need for ongoing support, it builds loyalty. Culturally intelligent leaders recognize that different people may need different kinds of help: perhaps a veteran employee only needs a couple of sessions to get back on track, but a new hire from a marginalized community – who maybe hesitated to seek help due to cultural stigma – might need a longer runway of support to truly thrive. The one-size-fits-all EAP approach doesn’t account for that nuance.
Beyond Session 4: Bridging the Gap with Therapist-Designed Solutions
Let’s be clear: none of this is about bashing EAPs. EAPs have saved lives and jobs; they were a revolution in their time. But supporting people at work in 2025 requires more. It requires acknowledging that our mental health challenges often outlast the support structures we’ve put in place. It’s about evolving from an old paradigm (“3 sessions and you’re done”) to a new one (“support is here whenever you need, in whatever form helps you most”).
Emotionally intelligent organizations are already moving this direction. They’re treating mental health not as a box to tick, but as a continuum. They’re training managers to spot burnout before it necessitates leave of absence. They’re offering things like “recharge days” or flexible schedules as systemic buffers against burnout. And they’re integrating therapist-designed tools that employees can trust – because they know these were built by people who get it, not by some random internet guru.
There’s even a bit of humor creeping into how progressive companies address these issues, and that’s a good thing. It breaks the ice. One company’s internal newsletter quipped, “Our EAP gives you 3 sessions; if you need a 4th, we’ve got [AppX] – like a therapist on your couch, minus the cat hair.” That got a chuckle, but it also opened employees’ eyes that, hey, there’s something after session 3! A better way doesn’t have to be dry or overly earnest; it can be warm, even funny, as it invites employees to engage. After all, laughter is a form of resilience too (ever had a giggle in therapy at how absurd life can be? Therapists often say that’s a sign of healing).
Cultural intelligence plays a role here as well. Humor and storytelling can be calibrated to your audience. A joke about therapy might land well in one office culture and flop in another. Knowing your people – across different regions, backgrounds, and identities – is key. The core message remains universal though: we see you, we support you, and we’re not going to abandon you after the “allocated” help is used up.
An Invitation to a Better Way
Ultimately, this conversation isn’t about therapy or apps or days off – it’s about trust and humanity at work. When an employee hits “Session 4,” figuratively speaking, and finds support still waiting for them, a powerful message is sent: you matter beyond your output; we care about you, not just the problem you’re trying to solve. That kind of message fosters profound loyalty and engagement. It’s the difference between an employee who merely survives at work and one who can actually thrive.
So, what happens on Session 4? It doesn’t have to be nothing. It can be the start of a new chapter: maybe with a different kind of support, maybe with a peer mentor or a digital program, maybe with a continued relationship with a therapist through your insurance or a company-sponsored plan. Session 4 can be where an employee transitions from short-term coping to long-term growth. It can be where burnout begins to turn into breakthrough. But only if we, as leaders and organizations, build that bridge.
This is an invitation – not a sales pitch, not a mandate, but a heartfelt invitation – to reimagine how we support people at work. We have an opportunity to turn EAP’s limitation into a launching pad for something more enduring. By complementing the quick fixes with sustainable tools like Reframe Refuel (and others), we show our colleagues that we’re in it with them for the long haul. We acknowledge that mental health isn’t a one-time project; it’s a continuous journey, much like professional development or physical health.
When employees feel genuinely supported, they bring their best selves to work. They have the emotional energy to be creative, to collaborate, to navigate change and stress. They know that if they stumble, there’s a safety net – and not one that evaporates after a predefined number of uses, but one that will catch them as many times as needed. That sense of security is priceless. It builds a culture of trust that no glossy wellness brochure can replicate.
In the end, helping someone through Session 4 and beyond isn’t just an investment in them – it’s an investment in all of us. It’s how we build workplaces where people can be open about their struggles and confident about their support. It’s how we turn the rhetoric of “our people are our greatest asset” into reality. And yes, it’s how we get better performance and retention too (because a supported employee is a loyal, productive one – the ROI writes itself).
So let’s ensure that Session 4 does happen, one way or another. Let’s make sure that when the counselor says “This is our last EAP session,” the next sentence is, “…but here’s what we’re going to do to keep helping you move forward.” In that moment, we transform a dead-end into a doorway.
After all, the story of supporting mental health at work is still being written. Let’s write it with compassion, creativity, and the courage to go beyond the quick fix. 💙
“I’m so glad you’ve joined me on this journey. This is just the beginning, and I’d love for you to be a part of it. Let’s share, support, and grow together. Drop a comment below—I’d love to hear your thoughts. Let’s keep this conversation moving forward.”
“We all have the power to redefine how we live. Keep moving forward—on your terms, in your way.”
Sources
National Center for Biotechnology Information (NCBI). (2022). Profile of small employers in the United States and the importance of Employee Assistance Programs during the COVID-19 pandemic.https://pmc.ncbi.nlm.nih.gov/articles/PMC9412145/
Alma. (2024). Continuing care beyond your EAP benefits. https://support.helloalma.com/hc/en-us/articles/9317079660827-Continuing-Care-Beyond-Your-EAP-Benefits
Lyra Health. (2025). A new approach to the outdated EAP. https://www.lyrahealth.com/resources/new-approach-to-eap/
Binns, F. (2025). Intake Case Study [Internal clinical document]. Unpublished proprietary data.
Binns, F. (2025). Intake Case Study [Internal clinical document]. Unpublished proprietary data.
Meditopia for Work. (2025). EAP statistics and utilization rates in 2025. https://meditopia.com/en/forwork/articles/eap-statistics-and-utilization-rates
Meditopia for Work. (2025). Why only 5 percent of employees use their EAP. (Companion data set). https://meditopia.com/en/forwork/articles/eap-statistics-and-utilization-rates
Meditopia for Work. (2025). Barriers to EAP utilization: stigma, lack of awareness, mistrust. (Infographic). https://meditopia.com/en/forwork/articles/eap-statistics-and-utilization-rates
Lyra Health. (2025). Employee perceptions vs. employer intentions: The mental-health support gap. (Survey brief). https://www.lyrahealth.com/resources/new-approach-to-eap/
Lyra Health. (2025). 82 % of employers believe they support mental health—only 50 % of employees agree. (Pulse poll). https://www.lyrahealth.com/resources/new-approach-to-eap/
Nivati. (2024). Pros & cons of Employee Assistance Programs. https://www.nivati.com/blog/pros-cons-of-employee-assistance-programs
Nivati. (2024). Average EAP session length is 2.5 sessions: Why that matters for outcomes. (Data spotlight). https://www.nivati.com/blog/pros-cons-of-employee-assistance-programs
People Management. (2024, Dec 12). EAPs alone cannot solve employee mental-health problems, association says.https://www.peoplemanagement.co.uk/article/1801586/eaps-alone-cannot-solve-employee-mental-health-problems-association-says
Single Grain. (2025, May 3). The office comeback: Is remote work over? https://www.singlegrain.com/the-office-comeback/
Spill. (2024). 53 Employee Assistance Programme (EAP) statistics for 2024. https://www.spill.chat/mental-health-statistics/eap-statistics



